Healthcare 2.0: How Robotics and AI are Revolutionizing Clinical Workflows
Intuitive design is becoming an integral component of medical technology, following the consumer space, as a number of undercurrents converge: increasing burdens on clinical practitioners, growing demands on healthcare systems, and the advancing complexities of technology. Surgical systems, for instance, serve highly trained experts performing mission-critical tasks, so improving usability in this scenario would require novel user interfaces and design approaches. So let's explore some core aspects of exemplary surgical tasks and outline methods to promote intuitive operation and efficient workflows. Care providers are already subject to physically, cognitively, and emotionally taxing responsibilities as is. By investing in their well-being, we might also improve patient satisfaction, outcomes, and operational efficiency as well.
The Quadruple Aim
Back in 2008, Berwick et al. proposed a measure of healthcare performance around improving population health, supported by the contributing aims of patient satisfaction and operational efficiency. However, this framework increased documentation requirements as patient expectations grew and healthcare systems faced rising cost pressures. The burden of improving performance was ultimately placed on clinicians, whose needs were overlooked leading to the deterioration of provider experience and subsequent declines in all three performance criteria. Consequently, the fundamental role of personnel in the delivery of healthcare was acknowledged as an added dimension in the Quadruple Aim, upon which emerging technologies will be increasingly evaluated against.
Healthcare technologies have grown in complexity alongside broader innovation, as is evident in the history of bronchoscopy. With its invention in 1964, the introduction of endobronchial ultrasound in 1992, the integration of electromagnetic (EM) tracking in 2006, and the regulatory approval of robotic bronchoscopy in 2018, pulmonologists learned to use a new device, interpret ultrasound images, register devices to medical images, and operate robots—all while practicing complex medical specialties.
Numerous reports highlight the burdens of technology borne by clinicians. Primary care physicians, for example, dedicate 25–50% of their attention to a computer, even while tending to patients. Data entry, while ultimately beneficial, disrupts the workflow of care and diminishes practitioner satisfaction. Electronic health record systems are widely regarded as a costly technological failure, leaving its potential unfulfilled while contributing to an epidemic of burnout. Similar usability shortcomings can be found in surgical systems, yet technology continues to march forward due to engineering platform commoditization, industry consolidation, and the influence of consumer technology. Usability is thus of paramount importance in the next generation of healthcare innovation.
Usability in surgical technology
The Food and Drug Administration (FDA) offers advice on medical device usability based on general-purpose standards, including human factors (AAMI/ANSI HE 75) and usability engineering (ANSI/AAMI/IEC 62366). These recommendations emphasize the prevention of user error through mechanisms such as warnings, disambiguation, and design controls. This guidance assumes a baseline of cognitive ability to use a device, without regard to any cognitive strain incurred by its use. A broader definition of usability (see [1] and [2]) consists of the following attributes:
- Learnability: The amount of training needed
- Efficiency: The fluidly of task performance
- Memorability: Retention of the initial training
- Errors
- Satisfaction
Surgical workflows consist of highly trained tasks performed regularly, so efficiency and errors are the most applicable traits; learnability and memorability effects, meanwhile, can be amortized over time. We'll build on the FDA guidance and extend the concept of usability toward efficiency. In particular, we'll focus on cognitive efficiency because surgical tasks often involve fine motor control in response to rapid judgment. Alleviating cognitive load thus has the potential to improve overall efficiency, reduce mental fatigue, reduce judgment errors, and ultimately improve clinician satisfaction, an essential component of the Quadruple Aim.
Cognitive effort in surgical tasks
Surgery is both a physically and a mentally demanding undertaking, so developers should strive to reduce the cognitive footprint of prospective surgical technologies. In this regard, inspiration on usability may be drawn from design techniques commonly used in the consumer product domain. At the same time, it is important to note that surgery is distinguished from everyday experience in fundamental ways, including the highly trained nature of tasks and the critical role of expert judgment.
Cognitive friction
Cognitive friction includes the intermediate steps that ostensibly lead to a goal, yet detract from it at the same time; this property can subtly influence one to avoid the task or its tools. For the critical task of surgery, cognitive friction can increase cognitive load, impairing judgment and motor skills. One example is the setup calibration of navigated devices, which is widely regarded as a cumbersome routine. Canonically, the user maneuvers a tracked device to touch several fiducials in a prearranged order. They then hope that the sequence was performed satisfactorily, lest they have to repeat this seemingly arbitrary ritual. In this work, the generic calibration task is streamlined to a single swipe in an effort to reduce cognitive load, as shown below; it can furthermore make re-calibration a less burdensome process, affording clinicians more freedom in setup and workflow.
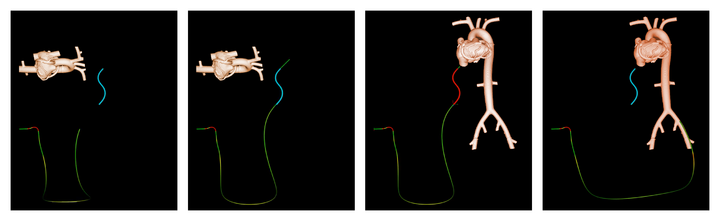
Beyond efficiency and convenience, reducing friction offers immediacy as a cognitive benefit.
A natural user tendency is to correlate the activation of a task with its eventual outcome in a bid to improve future results.
Reducing the latency of task execution allows one to infer cause-effect relationships more precisely, leading to improved performance and problem identification.
Reducing the number of steps to perform a task, especially one as well defined as calibration, can initiate inquiries into the division of labor between humans and machines. A shared responsibility scenario requires an intimate understanding of the task, a high level recognition of its progress, and interaction between users and systems. Further experiments can then evaluate the efficacy of various configuration options.
Natural vision
Medical images can be rendered in ways that are naturally interpretable. The figure below (Left) shows a 2D B-mode ultrasound image of a mitral valve. Standard 3D imaging (Center) helps reduce the cognitive load needed for mental 3D reconstruction. Then thanks to natural lighting and shadows, a photorealistic rendering (Right) improves depth perception and visualization of 3D spatial relationships, thereby reducing the cognitive effort of interpreting the arbitrary color shading more commonly applied in 3D ultrasound images. Natural visualizations may also reduce the need for robots designed to resolve hand-eye coordination challenges (e.g, this autonomous surgical snake).
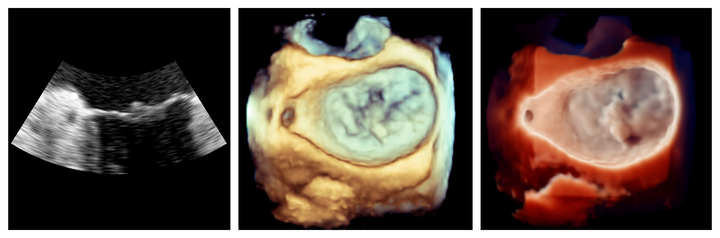
Artificially representing data for compatibility with human vision invites questions on the fidelity of the reconstructions, which will likely need to be tuned for different clinical applications.
Ergonomics
As technology is added to already crowded interventional labs, physicians strain to work around equipment. Augmented reality (AR) enables a paradigm shift in room design in which the tools revolve around physicians, providing them with the right content at the right location and time, as illustrated below. Immersing physicians in a tailored AR environment allows them to see the real world superimposed with the live imaging and data needed to guide precision therapy. Voice recognition, eye tracking, and gestures allow for easy interaction with interventional systems, keeping physicians' focus on patients rather than on technology. There is a vast solution space in augmenting a surgeon's reality, calling for an improved understanding of the effective use of the technology.

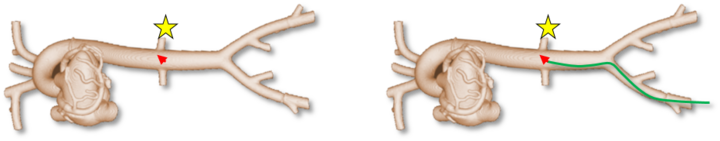
Spatial orientation
A robot can navigate a workspace given a point on its end effector—this singular point is often regarded as synonymous with the physical end effector itself. A clinician can likewise navigate a device in this manner, e.g., an EM tracked catheter. However, visualization of the entire device can make this task more intuitive, as pictured below. One possible explanation is that peripheral cues inform a mental model of the device, allowing for closure between expected and actual behavior. Small field-of-view imaging (ultrasound and endoscopy for example) provides further insight into the challenges of navigating with limited spatial context. Novel technologies will need to be developed to enlarge perspectives that would otherwise be hidden.
Linearity
As linearizing complex problems affords practical, if imperfect, solutions, linearizing the behavior of a technology can help users adjust to its imperfections. For example, a user can gainfully teleoperate a robot with low absolute accuracy provided the relationship between control input and actuation output is proportional and predictable. People excel at estimating linear trends, opening the possibility of relaxing technical requirements. Considerable engineering ingenuity may be needed to recast technological imperfections onto a linear scale.
Recap
The experience of clinical practitioners is vital to improving care delivery, especially as the demands on healthcare systems continue to grow. The usability of supporting technologies will thus increase in prominence as they become more advanced. In this article we outlined how complex systems can use intuitive interfaces to ease the burdens that technology otherwise imposes on clinicians. Examining various clinical innovations, a recurring observation is that an intimate understanding of users and workflows is a prerequisite to crafting suitable usability enhancements. The complexities of professional healthcare writ large call for thorough technical underpinnings, creative problem solving, and continuous improvements that emerge through experience.
This article was brought to you by P. Thienphrapa, B. Mory, A. Panse, V. Pai Raikar, A. Torjesen, and D. Schulman and appeared at the IEEE International Conference on Robotics and Automation (ICRA) Industry Forum during their memorable time together at Philips.
Related reading
- Top Medical Robotics Engineers Share 5 Key Lessons
- Interactive Endoscopy: A Next-Generation, Streamlined User Interface for Lung Surgery Navigation
- User-Centric Device Registration for Streamlined Workflows in Surgical Navigation Systems
- 10 Interesting Facts about the da Vinci Research Kit (dVRK)
- The Making of the da Vinci Research Kit (dVRK)
